Early Detection of Breast Cancer Cures Breast Cancer
Table of contents

There’s an overused phrase that’s been thrown around for decades and has now lost its meaning – “the cure for cancer“. That’s because nobody can agree on what that actually means. On one side, you have people who suggest that a cure for cancer has existed all along, but big pharma keeps it under the sheets because cancer is big money – like in 2015 – when spending on cancer drugs world wide exceeded $100 billion. Then the other side, which thinks that there is no single cure for the over 100 different types of cancers out there. That’s because “each person’s cancer has a unique combination of genetic changes” according to the National Cancer Institute which goes on to say that “40 percent of men and women will be diagnosed with cancer at some point during their lives”.
What both sides have in common is that they’re still searching for a cure for cancer – well, everyone except the millennial generation:

While it appears that today’s millennials appear to be taking more interest in a hipster breakfast item than a disease that fcuking kills you, these two things do have something in common. Cancer, like avocado toast, is something we could all do with a little less of.
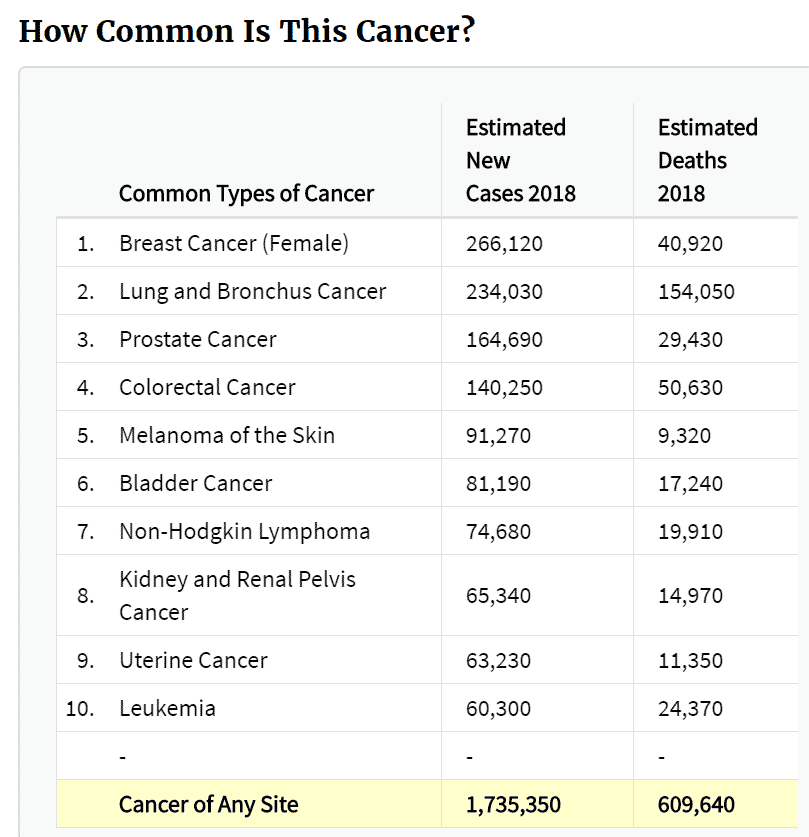
Then there are those of us who believe that while we can keep holding fundraisers and handing out pink ribbons in hopes of “finding a cure”, the low hanging fruit here is “early detection”. Speaking of pink ribbons, the reason why breast cancer seems to attract more attention than any other type of cancer is because of how relatively common it is:
According to Cancer Research UK, “more than 90% of women diagnosed with breast cancer at the earliest stage survive their disease for at least 5 years compared to around 15% for women diagnosed with the most advanced stage of disease.” That’s still not overly compelling, and doesn’t contain sufficient detail. For that, we turn to a man named Dr. Gabriel Hortobagyi whose accomplishments in the field of breast cancer research led him to write a paper on “The curability of breast cancer: present and future“. In that paper we learn something remarkable.
The Cure for Breast Cancer is Early Detection
The cure for breast cancer has been in front of our faces all along. The below excerpt was taken from Dr. Hortobagyi’s paper on breast cancer “curability” :
Perhaps the best source for this information is derived from long-term, prospective follow-up of the clinical trials of screening mammography [31]. With follow-up now exceeding 20 years, the Two County Trial reports very high survival rates, in the range of 96–98%. Similarly, patients with T1a+b N0 primary breast cancers diagnosed and followed as part of the same study had a 20-year survival that exceeded 85%. Another paper reported for this same group of patients a 40-year disease-specific survival rate of 80% or more [33]. Clearly, in both Stage 0 and Stage I, patients die of multiple other causes, but breast cancer is a cause of death for only a minority of patients. Personal cure is achieved for the great majority, and statistical cure is accomplished after 20 years or so.
What this seems to say is with early detection (Stage 0 or Stage 1), “personal cure is achieved for the great majority” who die of multiple other causes, just not breast cancer.
So, what do we mean by “early detection”? Breast cancer is detected by a variety of ways, the most popular being imaging or by self examinations. Here’s a look at the various imaging techniques being used:
While artificial intelligence is now said to be reading mammograms with a 99% accuracy, mammograms don’t always work though because of something called breast density which we wrote about before. In any case, it doesn’t seem like women are getting tested as often as they should. This begs the question, “How fast does breast cancer grow?”
How Fast Does Breast Cancer Grow?
If breast cancer grows very slowly, then once-a-year testing might be appropriate. However, according to what the experts say, by the time you feel that lump in your breast it’s already 2-5 years old. Since Medicare currently reimburses one mammogram a year, it seems like women should be fine than just getting tested yearly. On the other hand, do you really want to take that chance? Once a year seems low, especially considering these fascinating insights on tumor growth from Providence Health:
With most breast cancers, each division takes one to two months, so by the time you can feel a cancerous lump, the cancer has been in your body for two to five years. It can certainly seem like a lump appeared out of nowhere – especially if you or your doctor have recently examined your breasts and not felt anything suspicious – but in reality, the cancer has simply doubled that one last time necessary to be noticeable. By the time you can feel it, a breast tumor is usually a little more than one-half inch in size – about a third the size of a golf ball.
The key takeaway here is that most breast cancer tumors double in size every 1-2 months. Do you really want to be just finding out about your cancer when you feel some peanut-shaped growth in your breast on a Saturday afternoon before taking the kids to soccer? Wouldn’t it be so much better if that problem could be discovered in front of a health professional who can emphasize how benign the problem is because it was detected early?
Women need to get tested more often, and that’s something that Volpara Technologies is betting on with their business model. However, the winning formula will be to create a breast cancer test that’s easy for women to take, and doesn’t involve pulling out the twins in a freezing cold doctors office. What about an at-home breast cancer test that you could purchase via subscription so that you were tested every three months? At the moment, such a test doesn’t exist but we’re making some good progress with blood tests that detect breast cancer.
Cancer Blood Tests for Breast Cancer
We’ve talked before about Circulating Tumor Cells (CTCs) which can be detected in blood samples and offer a convenient way for us to develop “cancer blood tests”. Companies like Illumina see the potential here, and have invested in startups like Grail – which is incidentally looking to IPO in Hong Kong instead of Wall Street. We talked about some of the other companies playing in this space in our article on “8 Blood Tests for Cancer Being Developed by Startups.”
While Grail mulls over where they want to raise even more capital, another startup is already selling “the first protein-based blood test of its kind to provide early and accurate detection of breast cancer.”

Based on the above chart, false positives result in around $2-3 billion of unnecessary costs, not to mention all the stress the patients need to go through. To address this problem, Provista Diagnostics has developed Videssa Breast, “the first blood test of its kind, to complement breast imaging and improve the accuracy in early breast cancer detection in women with abnormal or unclear imaging findings.” When using Videssa Breast, one out of three biopsies finds cancer as opposed to one out of six when using only imaging. That reduction in biopsies is a benefit to healthcare providers and patients alike.
Provista Diagnostics also has a pipeline of similar tests based on their ProteoMark technology, like a test for ovarian cancer. Talk about a need for early detection. According to the company, “almost 80 percent of cases are diagnosed at late stages and the disease carries the highest mortality rate in women’s cancers.” That’s why it’s next in their pipeline:
Conclusion
Now we have at least two ways for “early detection” of the most prevalent cancer there is today. While Medicare may cover one mammogram a year, it appears that women still are not getting tested as much as they should. According to Provista, “Around 69% of women over the age of 45 will undergo imaging tests for breast cancer about once every two years. It’s not a problem of money for most, since it costs about $312 extra per year to get a mammogram once every quarter. Just forgo some tall caramel Frappuccinos and you’ll have the money saved in no time.
If something comes up during an imaging test, now you can ask for more decisive information from a blood test like Provista. Since out-of-pocket costs for Provista are $647 as of 2017, it’s not at a price point where most people would be able to take it periodically for early detection. That’s why getting those mammograms is so important. With AI algorithms identifying breast cancer in mammograms accurately now, expect the cost of a bog-standard mammogram to plummet as we move towards automated mammogram booths. In the not-so-distant future, your toilet will give you a health report every morning when you relieve yourself and your fridge will sort it out with a custom smoothie. Until then, early detection appears to be the cure for breast cancer we’ve all been waiting for.
Sign up to our newsletter to get more of our great research delivered straight to your inbox!
Nanalyze Weekly includes useful insights written by our team of underpaid MBAs, research on new disruptive technology stocks flying under the radar, and summaries of our recent research. Always 100% free.

















